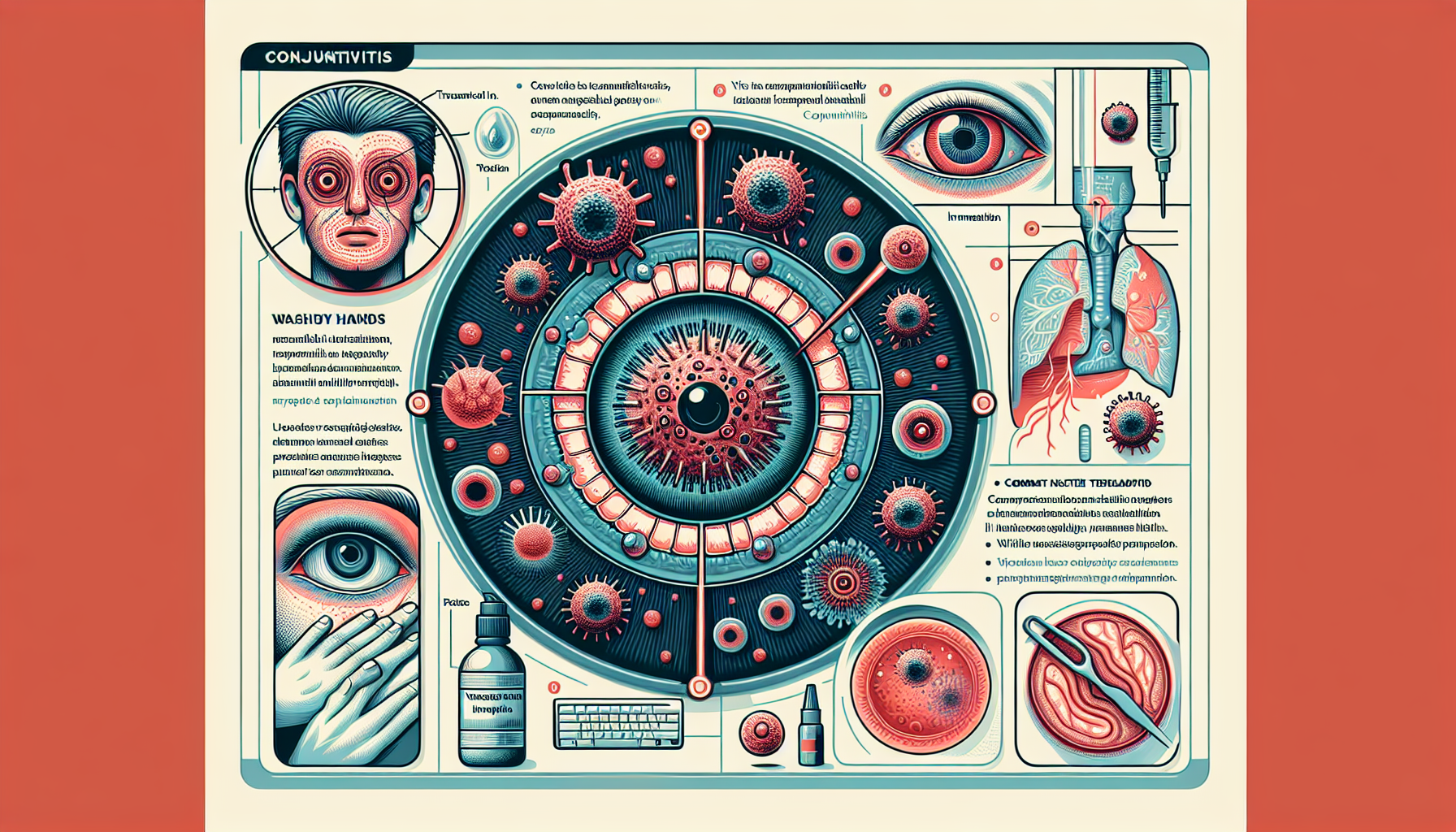
Viral conjunctivitis, commonly referred to as pink eye, is an inflammatory condition that doesn’t discriminate, affecting individuals from all walks of life. At the forefront of ocular ailments, it presents a set of symptoms that can disrupt daily routines and overall well-being. As we navigate through the complexities of this infection, it’s important to understand that the primary culprits are adenoviruses, although other viruses such as HSV and VZV also play a role. The high contagion factor of viral conjunctivitis is noteworthy, as it spreads rapidly through common actions such as hand-to-eye contact or exposure to respiratory droplets. Acknowledging the concern it raises, we are dedicated to not only addressing the uncomfortable redness, itching, and discharge associated with pink eye but also educating on effective prevention strategies.
In our pursuit of excellence in eye care, we recognize the importance of properly managing viral conjunctivitis. Typically resolving within 2 to 4 weeks, the condition does not usually demand specific treatment. However, being well-versed in the symptoms and adopting rigorous hygiene practices are pivotal in mitigating the spread. Through this article, we’ll dissect the intricacies of diagnosis, underscore the pivotal role of clinical features, and explore when laboratory tests could be advantageous. Armed with this information, we are poised to empower you with the best practices to tackle viral conjunctivitis head-on, ensuring that you or your loved ones are well-equipped to handle this ailment with confidence and ease.
Etiology and Pathophysiology
Understanding the underlying causes and the pathophysiology of viral conjunctivitis is fundamental for us to provide comprehensive care. The primary villain in the story of pink eye is the adenovirus, attributed to up to 90% of cases. Among the various types of adenoviral conjunctivitis, we encounter:
- Pharyngoconjunctival fever (PCF): Affects children and is caused by HAdV types 3, 4, and 7. It’s characterized by acute follicular conjunctivitis coupled with fever, pharyngitis, and swollen lymph nodes near the ears.
- Epidemic keratoconjunctivitis (EKC): The most severe form incited by adenovirus serotypes 8, 19, and 37 and known for its harsh symptoms and risk of corneal damage.
However, not all pink eye cases are courtesy of adenoviruses. Alternative viral culprits include: - Herpes simplex virus: Less frequent yet significant, causing herpetic conjunctivitis with follicular inflammation.
- Enteroviruses and picornaviruses: Minor players in the viral conjunctivitis scene, with picornaviruses EV70 and CA24v catalyzing Acute Hemorrhagic Conjunctivitis (AHC), notorious for its highly contagious nature.
- COVID-19: A recent adversary, implicated in conjunctivitis cases alongside more familiar respiratory symptoms.
As we delve deeper into the pathophysiology, pink eye reveals itself through either papillary or follicular conjunctivitis: - Papillary Conjunctivitis: Exhibits a cobblestone pattern of flattened nodules and is typically allergic in origin.
- Follicular Conjunctivitis: Characterized by dome-shaped nodules and commonly a response to infections, including viruses.
Clinical presentations for viral conjunctivitis patients can include: - Sudden onset of foreign body sensation, red-eye, itchiness, and watery discharge.
- Visual acuity that remains mostly unchanged.
- Red and possibly swollen conjunctiva with the potential of developing small, dome-shaped follicles.
The aptitude to diagnose viral conjunctivitis often relies on clinical judgment as laboratory testing such as adenovirus testing, with methods like cell culture and PCR, is usually reserved for cases that are protracted or when the diagnosis is uncertain. In terms of treatment, the goal is symptom alleviation, rather than eradicating the self-resolving infection. Symptom management may include: - Artificial Tears: For lubrication purposes.
- Topical Antiviral Agents: Primarily for herpetic conjunctivitis to reduce virus shedding.
It’s essential to differentiate pink eye from other conditions such as uveitis and systemic autoimmune diseases that can mirror its symptoms. The prognosis for viral conjunctivitis is predominantly favorable, with the majority of cases self-resolving within 14 to 30 days. Nevertheless, we must remain vigilant of complications like punctate keratitis and bacterial superinfection.
Each aspect of pink eye draws us closer to empowering our patients with the knowledge to manage their condition effectively. As one of America’s most common ocular problems, its economic and health impact cannot be understated, hence our commitment to shedding light on viral conjunctivitis with reliable, accessible information.
Symptoms and Signs
In identifying the hallmarks of viral conjunctivitis, also widely recognized as pink eye, it’s imperative to familiarize oneself with its distinctive symptoms which typically emerge as an unwelcome accompaniment to colds or other respiratory infections. As a professional eye care provider, we observe the following clinical manifestations:
- Burning Sensation: Patients often describe a discomfort akin to an irritant in the eye.
- Red Eyes: A conspicuous reddening of the whites of the eyes, which is the cornerstone symptom of pink eye.
- Watery Discharge: An abundant, transparent fluid that may crust over during sleep, signaling the body’s response to the viral presence.
The progression of viral conjunctivitis is marked by a highly contagious nature, becoming evident first in one eye and potentially affecting the other within several days. Our clinical experience aligns with the consensus that most episodes resolve spontaneously within 10-14 days.
For those seeking solace from the aggravating symptoms of pink eye, we recommend:
- Lubrication with Artificial Tears: These can be soothing and may assist in flushing out irritants.
- Cool Compresses: Apply these gently to the eyes to alleviate discomfort.
- Topical Medications:
- Corticosteroids: Consider these for severe cases marked by intense sensitivity to light (photophobia) or when visual clarity is compromised.
- Cyclosporin A Drops: These are an alternative if corticosteroid drops are contraindicated due to side effects.
- Professional Intervention: In extreme scenarios, the careful removal of any pseudomembranes by a specialist may be warranted to prevent long-term damage.
It cannot be overstated how pivotal preventive measures are in mitigating the spread of viral conjunctivitis. Anchored by stringent personal hygiene—avoiding hand-to-eye contact, frequent handwashing, and the use of individual towels and washcloths—these simple steps are our allies in curbing the transmission of pink eye. Our clinical judgment, augmented by diagnostic tools like NAAT when necessary, stands as our guiding principle to ensure that we are responding to each case of viral conjunctivitis with precision and care.
Diagnosing Viral Conjunctivitis
In discerning the presence of viral conjunctivitis, we prioritize a meticulous approach that aligns with our pledge to deliver comprehensive eye care. Recognizing viral conjunctivitis, colloquially termed pink eye, begins with a vigilant assessment of clinical signs complemented by an understanding of the patient’s ocular history and presenting symptoms.
- Clinical Diagnosis: As health practitioners devoted to your ocular health, our first step typically involves a thorough eye examination. We look for classical signs such as itchy eyes, redness, tearing, and discharge, which commonly appear in conjunction with upper respiratory ailments. Even though most cases of pink eye are self-limiting, lasting 2-4 weeks, this initial clinical assessment is vital to rule out other more serious conditions.
The infection route is also a critical factor in diagnosis, as viral conjunctivitis can spread through various means – accidental viral transfer from the hands to the eyes, direct contact with infected respiratory droplets, exposure to contaminated objects (fomites), or even swimming pools. Understanding these transmission pathways aids us not only in diagnosing pink eye but also in reinforcing preventive measures.
- Laboratory Tests: While the hallmark symptoms of pink eye often suffice for a diagnosis, certain situations warrant additional laboratory tests to confirm the viral etiology. When necessary, we may recommend:
- Conjunctival Cytology Smear and Giemsa Staining: A microscopic examination to detect viral inclusion bodies or changes in conjunctival cells.
- Culture: Although not routinely performed due to the self-limiting nature of viral conjunctivitis, a culture can identify specific viral strains when the infection deviates from the normal course.
- Rapid Immunoassays (AdenoPlus): A point-of-care test that offers quick results, particularly useful in detecting adenoviral infections.
We incorporate these diagnostic strategies as part of our arsenal to ensure a precise identification of the infection, which is paramount as the treatment of pink eye is primarily supportive in nature.
- Management and Prevention: Given the high transmissibility of pink eye, we emphasize preventive measures alongside symptomatic treatment. Promoting patient comfort involves:
- Cold Compresses: For alleviating discomfort and inflammation.
- Lubricants (Artificial Tears): To ease symptoms and potentially flush out viral particles.
Additionally, while severe itching may be relieved with topical vasoconstrictors and antihistamines, we advocate for a holistic approach centered around stringent personal hygiene:
- Frequent Hand Washing: The simplest yet most effective way to prevent spreading the infection.
- Avoidance of Shared Items: Personal items like towels, linens, and cosmetics should not be shared to curtail the risk of cross-contamination.
- Health Etiquette: Stay insulated at home and keep away from shared spaces such as workplaces or schools during active infection to curb the spread.
Understanding the difference in the course of viral conjunctivitis compared to bacterial forms is crucial. With viral infections tending to last around 2-4 weeks, patients can be reassured that their condition is typical and generally self-resolving. However, we remain vigilant for potential complications such as punctate keratitis leading to subepithelial infiltrates, which may arise and necessitate further intervention.
By approaching the diagnosis of pink eye with a comprehensive, evidence-based methodology, we reinforce our commitment to providing quality eye care that places patient comfort and wellbeing at the forefront.
Management Strategies
When managing viral conjunctivitis, our approach at the clinic is targeted towards alleviating discomfort and ensuring that our patients can continue with their daily activities with minimal disturbance. Here’s a detailed exploration of the strategies we employ:
- Symptom Relief: The mainstay of managing viral conjunctivitis, or pink eye, is providing symptom relief:
- Cold Compresses: To reduce swelling and provide a soothing effect.
- Artificial Tears: Serve as lubricants and help in flushing out irritants from the eyes.
- In cases of severe itching that disrupts daily life, Topical Vasoconstrictors and Antihistamines may be cautiously used, always considering their potential for local toxicity and hypersensitivity.
- Medication Applications: Specific medications are utilized for their respective benefits, taking caution to avoid complications:
- Topical Astringents or Antibiotics: These may be prescribed for patients at heightened risk for bacterial superinfection.
- Topical Steroids: Can be an option for treating pseudomembranes or vision-impairing subepithelial infiltrates. However, their usage is highly controlled due to risks such as exacerbating an underlying HSV infection and the possibility of creating a dependency on long-term treatment.
- For identifiable adenoviral infections, Povidone-iodine 0.8% is a potential remedy to decrease infectivity.
- Hygiene and Precaution Practices: To combat the highly contagious nature of pink eye, we stress the necessity of exemplary personal hygiene and precautionary practices:
- Hand Hygiene: Engage in frequent and thorough hand washing.
- Isolation Precautions: Patients should isolate for at least 2 weeks or until the redness and discharge from the eyes cease.
- Personal Item Care: Daily changing of towels and washcloths, avoiding the use of shared eye cosmetics, and meticulous contact lens care are all crucial steps.
- Professional Follow-up: We urge patients, particularly those prescribed medications, to adhere to follow-up care to monitor their recovery progress.
For specific viral causes of pink eye, like HSV or VZV, we may consider prescribing antiviral medications. These treatment options, along with our comprehensive hygiene education, aim to prevent the transmission of viral conjunctivitis and ensure our patients can navigate this temporary inconvenience with confidence and support.
It’s also essential for patients experiencing symptoms such as hyperacute conjunctivitis, suspect corneal involvement, significant visual loss, or suspected orbital cellulitis to consult with an ophthalmologist. Additionally, those whose condition does not improve with appropriate therapeutic measures should seek further evaluation to identify and address any underlying or associated issues.
Our priority is always the well-being of our patients, and we strive to provide personalized care that acknowledges and effectively addresses the nuances of each case of viral conjunctivitis we encounter.
Complications and Prognosis
While viral conjunctivitis, or pink eye, is generally a benign condition, we cannot overlook the potential for complications that, although rare, may be significant. As dedicated eye care professionals, our commitment to your health involves not only treatment but also education on the risks associated with pink eye:
Complications may include:
- Punctate Keratitis with Subepithelial Infiltrates: When the cornea is affected by fine, pinpoint deposits beneath its surface. This can lead to uncomfortable sensations in the eye and potential visual disturbances.
- Bacterial Superinfection: The initial viral infection may set the stage for secondary bacterial infection, which requires close monitoring and possible intervention with antibiotic treatment.
- Severe Dry Eye and Irregular Astigmatism: Resulting from alterations in the corneal surface, these conditions can impact both comfort and vision.
Notably, epidemic keratoconjunctivitis (EKC), a severe form of viral conjunctivitis, warrants special attention due to its associated risks, including: - Corneal Ulceration and Scarring: Leading to lasting changes in vision.
- Chronic Infection: Especially concerning for individuals with weakened immune systems.
The prognosis for most cases of pink eye is favorable, with the majority resolving without medical intervention within 7-10 days. However, infections resulting from HSV or VZV may present more complex challenges:
- These infections, while less common, demand a proactive approach given their propensity for inducing serious complications, and may necessitate the use of antiviral treatments.
Given this understanding, our preventative strategies are critical in safeguarding your ocular health:
- Strict Hand Hygiene: Diligent handwashing can drastically reduce the risk of both the spread and severity of pink eye.
- Avoidance of Contaminated Items: Ensuring personal items such as towels and eye makeup aren’t shared reduces potential exposure.
- Responsible Contact Lens Practice: Discontinuing lens wear during infection is crucial to avoid additional irritation and possible complication.
Lastly, it’s paramount to recognize the warning signs that may indicate developing complications:
- Should you experience symptoms such as eye pain, a sensation of something in your eye, blurred vision, or acute sensitivity to light, we encourage prompt evaluation to address any potential corneal inflammation or other adverse effects on your vision.
By maintaining a vigilant approach to both treatment and education regarding viral conjunctivitis, we aim to minimize the risk of complications while promoting swift and healthy recoveries for our patients.
Conclusion
In summary, our comprehensive review of viral conjunctivitis has allowed us to delve into its causative agents, with a special focus on adenoviruses, and touch upon the clinical signs and potential complications of this common eye condition. Through emphasizing symptom identification and the implementation of best practices in both hygiene and treatment, we have laid out an effective framework for managing and mitigating the impacts of pink eye on patients’ daily lives. The overview presented herein serves not only as a guide for healthcare providers but also as an educational resource for individuals seeking to understand and navigate the course of viral conjunctivitis with assurance.
The journey through understanding and handling viral conjunctivitis reinforces our recognition of the condition’s high contagion and the importance of early detection and prudent management. By adhering to the suggested preventive measures and considering further research or action when necessary, we can minimize both the spread and the duration of symptoms associated with pink eye. Ultimately, our collective adherence to informed strategies ensures the safeguarding of ocular health and the swift return to comfort and clarity for those affected by viral conjunctivitis.
FAQs
In our continued endeavor to elucidate the nuances of viral conjunctivitis, also widely recognized as pink eye, we address some of the most frequently asked questions on the subject:
What is the primary cause and how is it transmitted?
- Primary Cause: Viral conjunctivitis is primarily triggered by adenoviruses, akin to those causing the common cold, and is a prevalent condition especially among children under five.
- Transmission: Highly transmissible, the infection spreads swiftly in close-contact settings like daycare centers and schools. It is often accompanied by the telltale red or pink coloration in the whites of the eyes and may include watery discharge, a gritty sensation, or mild pain.
How is it diagnosed and what are the treatment options? - Diagnosis: Clinical observation of symptoms is the mainstay for identifying pink eye, with laboratory testing, such as PCR being highly specific, coming into play for persistent cases exceeding 4 weeks. The rapid AdenoPlus assay is available but less sensitive compared to PCR.
- Treatment Focus: We aim to assuage symptoms, recommending artificial tears for lubrication, cold or warm compresses for comfort, and promoting diligent hand hygiene to prevent further spread. For specialized cases involving HSV or VZV, topical antiviral agents are employed.
What should I know about the prevention and management of complications? - Preventing Spread: The infection typically abates within 2 to 3 weeks. Preventive practices include regular handwashing, not sharing personal items, and for contact lens users, abstaining from wearing lenses until fully recovered.
- Managing Complications: For more severe consequences, like subepithelial infiltrates causing significant visual issues, immunomodulating eye drops like tacrolimus or cyclosporine A have proven effective. With the high infectivity rate of viral conjunctivitis, especially forms like Acute Hemorrhagic Conjunctivitis and those linked to COVID-19, isolation is advisable to mitigate the economic and health impact.
As we continue to confront the challenges posed by viral conjunctivitis, our unwavering commitment remains to provide you with authoritative, accessible insights into its management and prevention. Whether navigating the nuances of personal hygiene to thwart its transmission, or understanding the implications of various treatment modalities, we’re here to support you in achieving the best possible outcomes for your ocular health.


Worksite
All Employees Served With Direct Vision Care All In One Day At Their Worksite!.
Glasses2Classes
Vision screenings, eye exams, and eyewear for all students at their schools!
Community Events
Provide Easy Access To Eye Care & Eyewear for Your Entire Community!
At Home
Skip the trip! We travel directly to all fragile homebound patients!